Everyone has the right to make decisions about health treatment they receive from a health care provider.
All adults are presumed to have capacity to consent to health care unless there is evidence of impaired decision making capacity.
The Health Care Decision Making Act 2023 addresses the gap in Northern Territory law concerning health care decision making for people who have lost some or all of their capacity to make their own health care decisions. It also governs the provision of urgent health care without consent to adults and children following the repeal of the Emergency Medical Operations Act 1973.
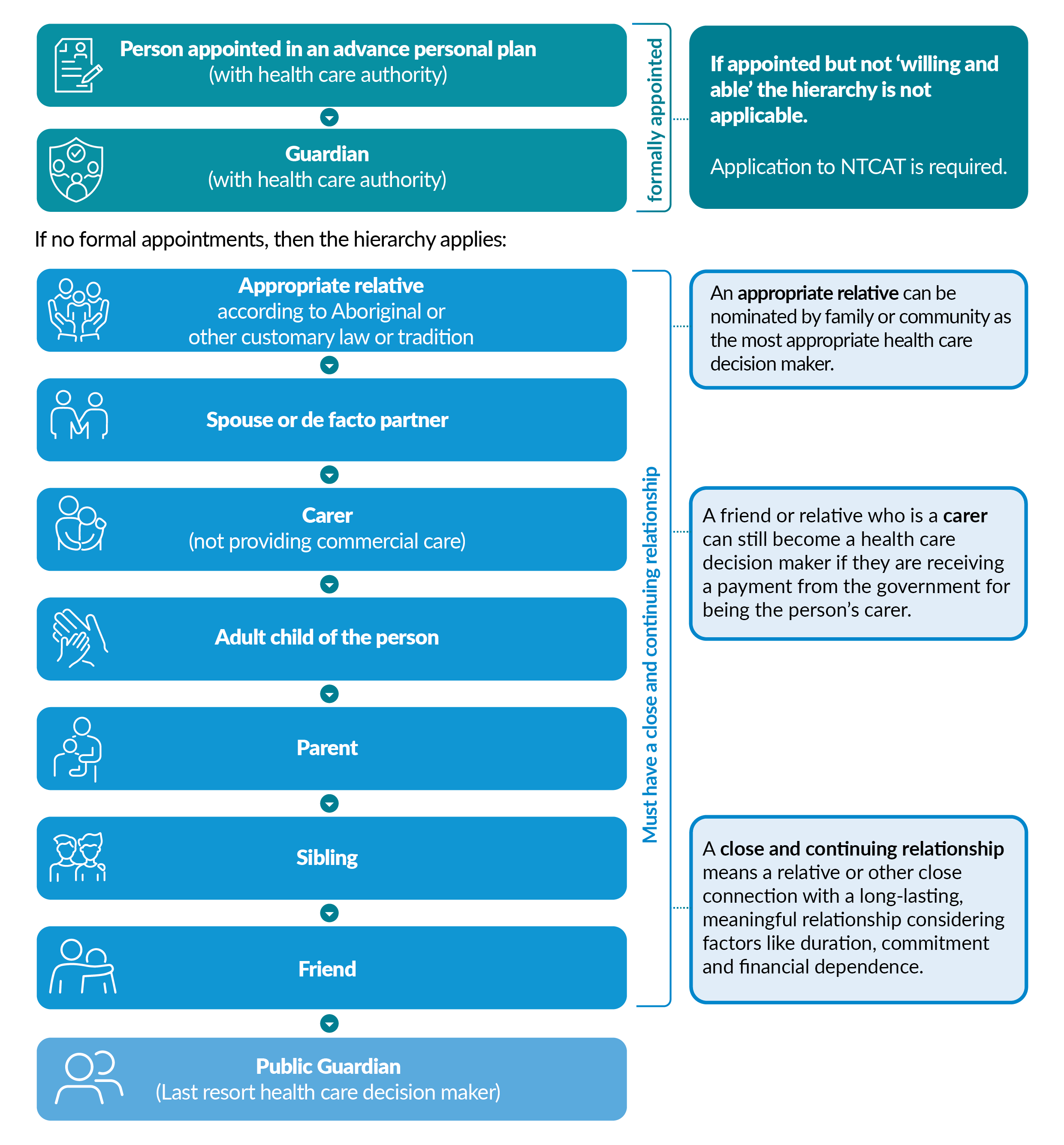
The Act establishes a hierarchy of possible health care decision makers including family and close friends, including formal recognition of First Nations kin who can lawfully provide consent on behalf of the patient.
What health care is included?
Health care is broadly defined as any kind of health care, including the following services or anything provided as part of the following services:
- Any health service provided by a registered health professional;
- Hospital services;
- Mental health services;
- Pharmaceutical services;
- Ambulance services;
- Community health services;
- Health education services;
- Welfare services necessary to implement health services;
- Pathology services;
- Allied health services;
- Assessment conducted by a health care provider (such as an aged care assessment)
When is a health care decision maker required?
When a person’s ability to make a health care decision is impaired, they may need someone to make a health care decision on their behalf.
This person is known as their health care decision maker. This role is specific for the health care decision needed at the time. A health care decision maker is not permanently appointed unless by a legal appointment such as a Guardianship order, or under an Advanced Personal Plan.
A health care decision maker is needed when:
- A person has impaired capacity to make a decision about the health care needed;
- The person has not made an advanced consent decision in their Advanced Person Plan about the health care needed;
- The health care is significant (implied consent cannot be accepted from the person); and
- The person is not likely to regain capacity within a reasonable timeframe to enable the health care needed.
Refer to our flowchart Adult Health Care Consent for more information.
What is impaired decision making capacity?
An adult is presumed to have capacity to make a health care decision unless there is evidence to the contrary. An adult patient who merely appears to have impaired decision making capacity is still presumed to have capacity to consent.
An adult patient is still presumed to have capacity to consent, even if they have a disability, need support to communicate, understand information or to make decisions;
Even if an adult has or is suspected to have impaired decision-making:
- They can still give consent if their impairment doesn't affect the specific decision. (A person might struggle with some decisions but not others.)
- If their decision making ability is expected to improve soon, it's better to wait and get their consent before proceeding with treatment.
Refer to our flowchart Adult Health Care Consent for more information.
A person may have impaired decision making capacity if they have difficulty:
- Understanding and retaining information relevant to the health care decision;
- Weighing information relevant to the health care decision in order to make the health care decision;
- Communicating the health care decision in some way;
- Understanding the effect of the health care decision.
Decision making capacity is:
- DOMAIN SPECIFIC – a person may be able to make health care decisions but not financial decisions
- DECISION SPECIFIC – a person may be able to make some health care decisions but not others (e.g. may be able to consent to a blood test but not to a course of cancer treatment)
- TIME SPECIFIC – a person’s capacity may fluctuate (e.g. they might have better cognition at certain times of the day or regain capacity at a later date)
Our guideline ![]() Determining decision making capacity for a health care decision provides more information on impaired decision making capacity.
Determining decision making capacity for a health care decision provides more information on impaired decision making capacity.
Hierarchy of Health Care Decision Makers
People in the Hierarchy of health care decision makers are potential health care decision makers, listed in order of priority.
The first two options are appointed under legislation. The remaining options have familial or other connections to the patient and must have a close and continuing relationship with the person.
Where there is no other option the Public Guardian has authority to make health care decisions as a last resort.
See our ![]() Guideline – Determining the appropriate health care decision maker for more information
Guideline – Determining the appropriate health care decision maker for more information
Determining the most appropriate health care decision maker
The appropriate health care decision maker is the person on the hierarchy who meets the following criteria at the time the decision is needed (note, this may not be the same person each time a decision is needed);
- Is the option that holds the highest priority under the Hierarchy of health care decision makers
- Is an adult and
- Is ‘willing and able’ to make the decision.
When there is more than one appropriate health care decision maker on the same level of the Hierarchy of health care decision makers such as multiple adult children, the following approach should apply wherever possible:
- Ask the patient who they would prefer to make the health decision for them;
- Consider how ‘close and continuing’ the relationships are with the person;
- Parties could act together;
- Parties can nominate a health care decision maker amongst themselves where the chosen party is an option on the hierarchy (delegating responsibility to someone else not listed on the hierarchy is not permitted).
If there is disagreement about the health care decision or nominating a health care decision maker, an application to NTCAT is required to determine the appropriate decision maker. The application must be made by an interested party (including the health care provider).
Refer to our guideline ![]() Determining the appropriate health care decision maker for more information.
Determining the appropriate health care decision maker for more information.
How to make health care decisions
Before making a decision for the person, a health care decision maker should try their best to help them make their own decision, using any available support suitable for the situation.
Support to assist the person in making the health care decision could include:
- Using information or formats tailored to the particular needs of the person;
- Access to a language or Auslan interpreter;
- Using modified language, visual aids or other means;
- Communicating or assisting the person to communicate the person's decision;
- Giving the person additional time and discussing the matter with the person;
- Using technology that alleviates the effects of the person's disability.
If the person isn’t able to make their own decision with support, a health care decision maker must follow the below steps, preferring each option before progressing the next.
- If the persons has an ‘advance care statement’ in their Advance Person Plan that provides their wishes relevant to the health care decision needed, then the health care decision maker must make a decision that aligns with those views.
- If the person doesn’t have an advance care statement, the health care decision maker must make the decision that the person would have wanted.
- If the health care decision maker doesn’t know what the person would have wanted they must make a decision in the person’s ‘best interest’.
Refer to our guideline ![]() Making health care decisions for more information.
Making health care decisions for more information.
What happens if the person has no one on the hierarchy?
In an emergency or for ‘![]() routine’ health care treatment that the person is agreeable to, the doctor or other health care provider is allowed to proceed with treatment without the consent of the health care decision maker.
routine’ health care treatment that the person is agreeable to, the doctor or other health care provider is allowed to proceed with treatment without the consent of the health care decision maker.
The Public Guardian has authority to make health care decisions as a last resort where:
- The person has impaired decision making capacity for the specific health care decision needed; and
- The person has not made an advance consent decision in an Advance Personal Plan in relation to the health care needed; and
- There are no identified health care decision makers willing and able to make the decision; or
- The appointed Guardian or Advanced Personal Plan decision maker is not willing and able to make the decision and an application to NTCAT has not been made; or
- The Public Guardian is ordered to be the health care decision maker by NTCAT.
Requests to the Public Guardian to make a health care decision in these instances can be made by completing the ![]() Health care decision request form to be submitted by email to pgt.health@nt.gov.au.
Health care decision request form to be submitted by email to pgt.health@nt.gov.au.
Please see the ![]() Health care decision requests process for a step-by-step guide to requesting health care decisions from the Public Guardian.
Health care decision requests process for a step-by-step guide to requesting health care decisions from the Public Guardian.
Before requesting assistance from the Public Guardian, please review our flowchart, Adult health care consent to ensure you have explored all other options and fulfilled your responsibilities as a health care provider. Specifically there is the requirement to:
- Check if the person has already made an advance consent decision in an Advance Personal Plan (APP) regarding their current health care needs.
- If there is no known advance consent decision after reasonable efforts were made to determine this, contact the appropriate health care decision maker for the adult with impaired decision-making capacity.
- Determine whether the person is subject to a Guardianship Order in relation to health care.
- Determine the person’s capacity to make the specific health care decision needed.
Refer to our guidelines ![]() Initial responsibilities of a health care provider and
Initial responsibilities of a health care provider and ![]() Determining impaired decision making capacity for a health care decision for more information.
Determining impaired decision making capacity for a health care decision for more information.
What decisions can a health care decision maker make?
Health care decision makers cannot make decisions about all types of health care in all circumstances.
Health care decisions are made at the time the health care decision is needed and could be for a single treatment or as a course of health care to be provided over a period of time.
Health care decision makers do not have authority to consent to:
- Restrictive practices (There are certain exceptions to this. Refer to the NT Health website for further information)
- Restricted health care (This requires an application to NTCAT)
Restricted health care includes:
- Sterilisation*
- Termination of a pregnancy*
- Removal of non-regenerative tissue
- Special medical research or experimental health care
- Health care not yet accepted as evidence-based
- Electroconvulsive therapy
- Treatment involving adverse stimulus
* Note that in some circumstances a health care decision-maker can consent to sterilisation and the termination of pregnancy. Please contact us if you require further clarification.
If a health care decision maker is not available, then the health care provider can provide the health care without consent only in the following circumstances:
- The health care is ‘routine’ – When the person is not objecting to health care that doesn’t cause significant intrusion, risks, side effects, pain or distress including personal care and grooming. Refer to our guideline,
 Routine health care for more information.
Routine health care for more information. - An emergency – when the person needs to be treated urgently to save their life of prevent them from serious damage to their health, or significant pain or distress;
- Relief from pain and distress – in the context of palliative care and preventing a person from needlessly suffering. A decision to stop active treatment and progress to a palliative care plan is made by the health care decision maker in consultation with the treating team. However, a health care decision maker cannot refuse health care that would to prevent unnecessary pain or suffering to the person.
What if I have concerns about a health care decision maker?
If a health care provider believes a health care decision maker is not fit or able to make the health care decision an application must be made to NTCAT to determine:
- who should be the health care decision maker or
- make the health care decision
If a health care decision maker is:
- Refusing to consent to ‘significant’ treatment for a patient with impaired decision making capacity
and
- Does not know, and cannot infer, the wishes and views of the patient with impaired decision making capacity.
An interested party must apply to NTCAT (unless not reasonably practical to do so) to;
- Determine who should be the health care decision maker; or
- Make the health care decision.
The health care provider must provide written notice to the Public Guardian in relation to this matter using the form ![]() Report to the Public Guardian regarding a health care decision maker.
Report to the Public Guardian regarding a health care decision maker.
Refer to our guideline, ![]() Determining the appropriate health care decision maker for more information.
Determining the appropriate health care decision maker for more information.
Supporting Guidelines
The Public Guardian has published the following guidelines to be followed by health care providers and health care decision makers.
Pursuant to Section 55 of the Health Care Decision Making Act 2023, a health care provider must make reasonable efforts to follow these guidelines.
 Adult health care consent flowchart
Adult health care consent flowchart Initial responsibilities of a health care provider guideline
Initial responsibilities of a health care provider guideline Determining decision making capacity for a health care decision guideline
Determining decision making capacity for a health care decision guideline Determining the appropriate health care decision maker guideline
Determining the appropriate health care decision maker guideline Hierarchy of health care decision makers
Hierarchy of health care decision makers Making health care decisions guideline
Making health care decisions guideline Health care decision request process
Health care decision request process Routine health care guideline
Routine health care guideline
For more information or clarification on any content contained within these documents please contact us.
